Introduction: Studies have shown that transfusion-dependent (TD) patients with MDS have worse overall survival (OS) than transfusion-independent (TI) patients. However, few studies have examined physicians' perspectives on the relationship between transfusion dependence and OS and other clinical and economic outcomes in MDS. The current study investigated physicians' understanding of the impact of transfusion status (TS) on clinical and economic outcomes in 5 European countries.
Methods: Interviews were conducted with physicians (3 each in France, Germany, Italy, Spain, and the UK) to pre-test and revise the study questionnaire, a 40-minute web-based physician survey via the M3 Global Research physician panel, for relevance and understanding. The revised questionnaire was translated to allow physicians to complete the survey in their native language. To participate in the survey, physicians had to be specialized in oncology/hematology, have been in practice for 2-35 years, spend ≥ 75% of their time in direct patient care, and have managed ≥ 15 patients with MDS in the past 3 months. The survey asked physicians for their perspectives on the impact of TS on risk of death, acute myeloid leukemia (AML) progression, chance of leukemia-free state (LFS), significant bleeding events, number of infection events, hospitalizations, and ER visits, based on their own clinical experience, beliefs, and knowledge of the literature. In the instructions accompanying the survey, physicians were provided with a definition of transfusion dependence (≥ 1 unit(s) every 8 weeks), transfusion burden (TB; high burden: ≥ 4 units every 4 weeks), and MDS International Prognostic Scoring System (IPSS) and revised IPSS (IPSS-R) risk levels to ensure consistency across all physicians. All results were reported descriptively, with frequency counts and percentages for categorical/ordinal data and mean (standard error [SE]) for continuous data.
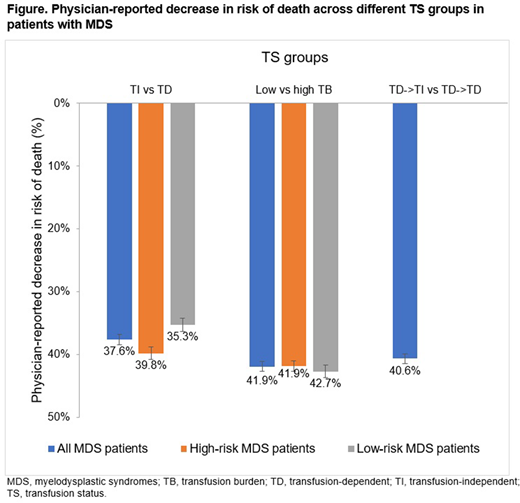
Results: Overall, 244 hematologist/oncologists, 124 hematologists, and 10 oncologists completed the survey in France, Germany, Italy, Spain, and the UK (n = 75 [approx.] in each country). On average, physicians were in practice for 14.70 years (SE 0.32), 41.3% were between the age of 45 and 54 years, and 64.3% were male. Physicians had seen an average of 54.5 patients (SE 2.26) with MDS in the past 3 months. The average risk of death among TI patients versus TD patients was 35.27% (SE 1.06) lower in the lower-risk MDS population and 37.61% (SE 0.87) lower among patients of all risk levels. The average risk of death among patients with low versus high TB was 42.65% (SE 0.95) lower among lower-risk TD patients and 41.89% (SE 0.75) lower among all-risk TD patients. The average risk of death for TD patients who became TI after treatment was 40.64% (SE 0.79) lower than for those who remained TD after treatment, across all risk levels (Figure). Similar results were found for AML progression and chance of LFS with TD patients having worse outcomes. The mean number of infection events per person per year (PPPY) was reported to be 3.96 (SE 0.82) for lower-risk TI patients and 5.15 (SE 0.91) for lower-risk TD patients, and the mean number of significant bleeding events PPPY reported was 2.88 (SE 0.85) for lower-risk TI patients and 3.46 (SE 0.81) for lower-risk TD patients. The mean number of all-cause hospitalizations PPPY reported was 3.62 (SE 0.76) among TI patients and 6.35 (SE 0.89) among TD patients. Physicians also reported TI patients having 3.28 (SE 0.84) ER visits PPPY and TD patients having 5.61 (SE 0.84) ER visits PPPY. These findings were numerically similar across all 5 countries.
Conclusions: Overall, physicians reported a greater risk of death, AML progression, and leukemic death, more infections and significant bleeding events, and increased hospitalization and ER visits for patients with MDS who are TD versus TI, based on their clinical experience and knowledge of the literature. The results were similar across patients with different risk levels and across the countries in question. New treatment options for patients with MDS to reduce or eliminate TB are warranted.
Kulasekararaj:Alexion Pharmaceuticals Inc.: Honoraria, Membership on an entity's Board of Directors or advisory committees. Gupta:Kantar: Current Employment; Bristol Myers Squibb: Consultancy, Research Funding. Constantino:Kantar: Current Employment. Grisolano:Kantar: Current Employment; Bristol Myers Squibb: Consultancy. Tang:Bristol Myers Squibb: Current Employment; Asclepius Analytics: Current Employment. Jones:Bristol Myers Squibb: Current Employment. Tang:BMS: Current Employment, Current equity holder in publicly-traded company.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal